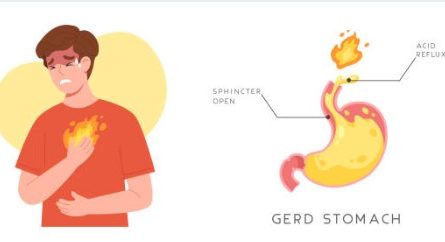
Acid reflux, also known as gastroesophageal reflux disease (GERD), is a medical condition that occurs when the stomach acid flows back into the esophagus. The esophagus is the tube that carries food from the mouth to the stomach. Normally, a ring of muscle at the lower end of the esophagus called the lower esophageal sphincter (LES) prevents stomach acid from flowing backward.
Acid reflux, or gastroesophageal reflux (GER), can cause a range of symptoms that vary from person to person. Here are some common symptoms associated with acid reflux.
Heartburn
A burning sensation or discomfort in the chest that typically occurs after eating, especially when lying down or bending over.
Regurgitation
The backflow of stomach contents, including acid and undigested food, into the throat or mouth, resulting in a sour or bitter taste.
Chest pain
Some individuals may experience chest pain or discomfort that can mimic the symptoms of a heart attack. It may radiate to the neck, jaw, or arms.
Difficulty swallowing (dysphagia)
A sensation of food getting stuck or difficulty swallowing, often accompanied by pain or discomfort in the chest or throat.
Chronic cough
A persistent dry cough, especially at night, that is often triggered by the reflux of stomach acid into the throat.
Hoarseness or voice changes
Acid reflux can irritate the throat and vocal cords, leading to hoarseness, a raspy voice, or voice fatigue.
Sore throat
Irritation and inflammation of the throat can cause a persistent sore or scratchy throat.
Laryngitis
Inflammation of the voice box (larynx) resulting in a hoarse voice, voice changes, or loss of voice.
Excessive saliva production
Some individuals may experience increased saliva production, often as a response to acid reflux and throat irritation.
Dental problems
Acid reflux can cause erosion of tooth enamel, leading to tooth sensitivity, cavities, or tooth decay.
It’s important to remember that not everyone with acid reflux experiences all of these symptoms. The severity and frequency of symptoms can vary from person to person. If you’re experiencing persistent or bothersome symptoms, it’s advisable to seek medical evaluation and guidance from a healthcare professional. They can assess your symptoms, provide an accurate diagnosis, and recommend appropriate treatment options to manage your acid reflux effectively.
When do I need medicine for acid reflux
You may need medicine for acid reflux if you experience frequent or severe symptoms that significantly impact your quality of life. Here are some indications that you may benefit from medication for acid reflux.
Frequent or persistent symptoms
If you experience acid reflux symptoms, such as heartburn or regurgitation, more than twice a week, it may indicate a need for medication. Occasional or mild symptoms can often be managed with lifestyle modifications, but if your symptoms are frequent, persistent, or increasingly bothersome, medication may be necessary.
Inadequate relief from lifestyle modifications
If you have made lifestyle changes to manage your acid reflux symptoms but find that they are not providing sufficient relief, medication may be helpful. Lifestyle modifications include dietary adjustments, avoiding trigger foods, weight management, elevating the head of the bed, and avoiding lying down after meals.
Disruption of daily activities
If acid reflux symptoms interfere with your daily activities, work, sleep, or overall well-being, medication can be considered to help alleviate the symptoms and improve your quality of life.
Complications of acid reflux
If you develop complications related to acid reflux, such as erosive esophagitis, Barrett’s esophagus, or respiratory issues, medication may be necessary to manage and prevent further complications.
It’s important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan. They can assess the severity of your symptoms, consider any underlying conditions, and recommend the most appropriate medication options for your specific situation. They will also consider other factors such as your medical history, potential interactions with other medications you may be taking, and any underlying health conditions you may have.